Patellar Tendinopathy aka Jumper’s Knee – for Basketball and Jumping Athletes
Monday, February 12, 2024
Patellar Tendinopathy aka Jumper’s Knee – Management Guide for Basketball and Jumping Athletes
Patellar tendinopathy, also known as “Jumper’s knee”, is a painful overuse condition affecting the patellar tendon. It tends to be a common condition with highly active individuals, particularly athletes participating in sports that involve repetitive jumping and sprinting such as basketball, volleyball and track and field athletes.
As an avid basketball player myself, I have experienced jumper’s knee and it almost always this tends to follow a period of training that involves significant volumes of intense jumping. Aside from the physical pain, I have personally experienced the frustrations of patellar tendon pain forcing me to reduce my basketball playing time. I personally hate not playing or training, which is why I endeavour to find the best exercise strategies to manage this frustrating condition to help myself and my patients who are also going through the same rehab journey.
How does patellar tendinopathy present?
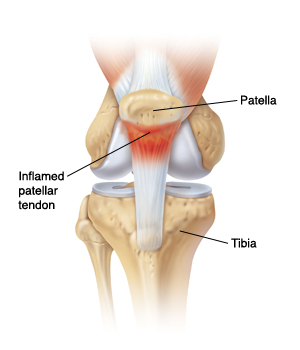
Pain tends to be worst with jumping and sprinting activities, activities such as squatting/lunging and other exercises that load the tendon are also provocative of pain.
It is important to differentiate patellar tendinopathy from other conditions that cause anterior knee pain such as patellofemoral pain syndrome, I always recommend all patients see an experienced physiotherapist or sports physician for an accurate diagnosis first before commencing exercise-based rehabilitation.
Causes of patellar tendinopathy
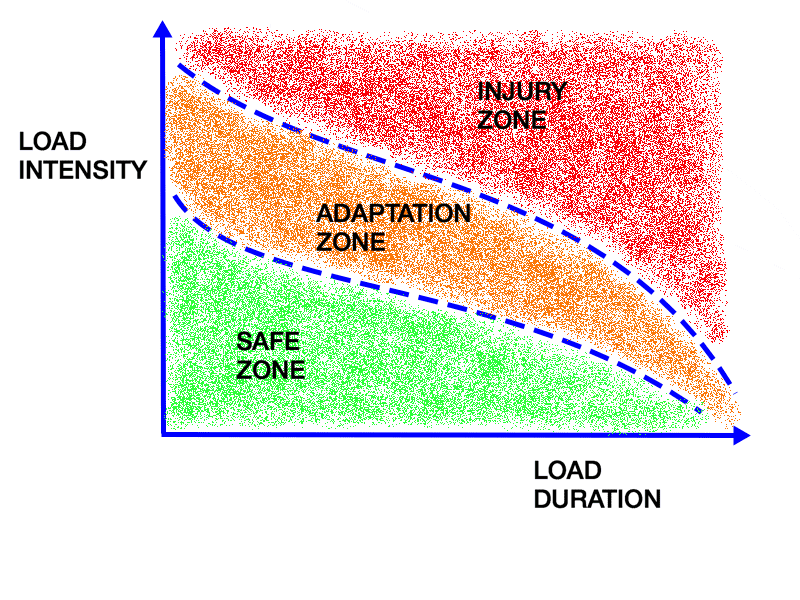
In most instances, patellar tendinopathy occurs following a period of rigorous exercise that loads the patellar tendon excessively. Typically, this involves high volumes of intense jumping. It can also occur in strength athletes such as CrossFit and Olympic lifting athletes who place significant demands on their patellar tendon through heavy squatting movements and other high velocity exercises that load the patellar significantly.
Additionally, deconditioning is a risk factor that can make individuals prone to exceeding their load tolerance. I myself experienced this very recently when I had a fractured wrist which led to some deconditioning and I attempted to return to jump training and basketball too quickly. The period of lower intensity training during my injury meant my patellar tendon was not experiencing a high degree of load, and as the saying goes “if you don’t use it, you lose it”. When I had returned to jumping, my tendon had lost load tolerance and was not prepared for the intense jump training I did, leading to an imbalance in load tolerance which resulted in developing tendinopathy.
Management of patellar tendinopathy
Managing activities that load the patellar tendon is arguably the most critical factor for management of patellar tendinopathy. This typically means temporarily ceasing or reducing the volume/intensity/frequency of athletic activities that provoke pain. In mild cases, this can just mean simply reducing how often you play sport or run/jump. Once training load has been reduced to a tolerable level, training load can be gradually increased over time as tolerated.
Exercise intervention is crucial for increasing the load capacity of the patellar tendon. There is evidence suggesting that isometric exercise is well tolerated by most individuals and is very effective for reducing pain associated with tendinopathies. Eccentric exercises and heavy slow resistance training are also shown to be equally effective exercise strategies to manage patellar tendinopathy.
How to manage pain
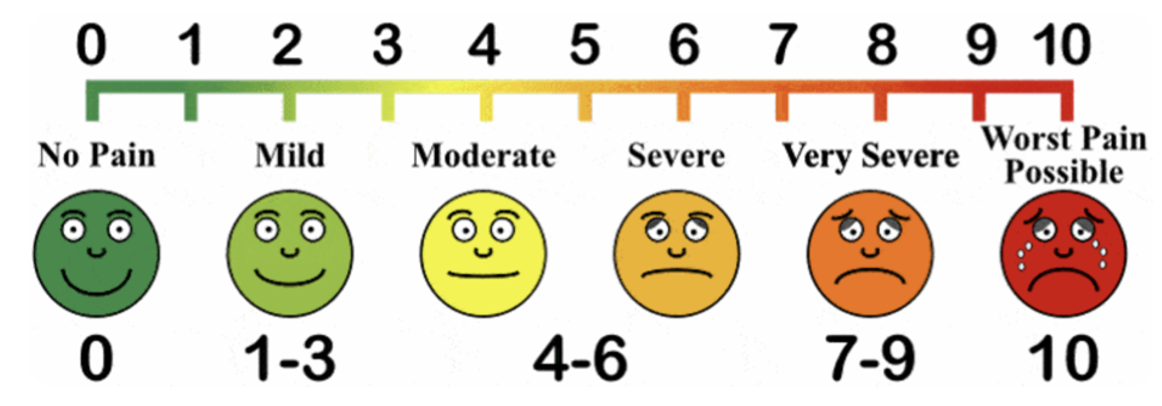
Experiencing pain during exercise-based rehab is normal and expected, finding strategies to keep pain tolerable while continuing to load the tendon is the goal.
The first strategy is reducing speed of movements, higher velocity activities (plyometrics, jumping, sprinting) are much more provocative of tendon pain, slower movements (heavy slow resistance, isometrics, eccentrics) tend to be less painful.
Reducing range of motion can also be useful, in the case of patellar tendon pain this would be reducing the angle of knee bend during squatting/lunging or other quadriceps exercises.
The experience of pain is a tricky topic as it can be an indicator that we are pushing too hard too soon, on the other hand it can also be a normal experience that doesn’t suggest we are causing more harm. To simplify things, I tend to advise that intolerable pain (which is subjective for each person) indicates that we need to regress exercises in some way.
Another useful indicator is that pain the following day is a better indicator than pain in the present moment. If pain is worse the following day, then that tends to be a good indicator that the training loads was excessive and should be regressed. In most cases, I tend to recommend pain stays below 3/10 following exercise.
Additionally, patellar tendon straps can be a useful short-term strategy to limit loads transmitted through the patellar tendon during provocative activities. While this is a useful strategy for in-season athletes, it should be used in conjunction with load management and exercise-based rehab strategies for long-term benefits.
Sample exercise protocol for patellar tendinopathy
Below is a sample isometric exercise protocol for managing patellar tendinopathy, this is a great starting point for most individuals that focuses on improving the load capacity of the patellar tendon. The progression and management of a rehab program for patellar tendinopathy is best guided by an experienced physiotherapist or exercise physiologist.
Daily Protocol
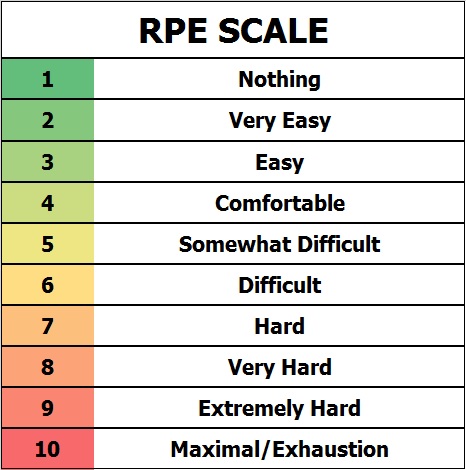
The below protocol uses rate of perceived exertion (RPE) to adjust how intense the exercise is. RPE simply means your perceived rating of how hard the set was from 1-10, with 1 being extremely easy and 10 being a maximal effort where you are unable to push further. Tendons are capable of tolerating extremely high loads, to stimulate them to adapt we need high intensity and loads.
To increase RPE, increase weight on the exercises or progress through the split squat variations to increase difficulty.
Warm Up
Bodyweight split squat, accumulate 2-3 minutes per leg using 2-4 sets at an RPE 6-7
Working Sets
Split Squat Isometric – 2 sets per side x 30-45 seconds, RPE 8+
Leg Extension Isometric – 2 sets per side x 30-45 seconds, RPE 8+
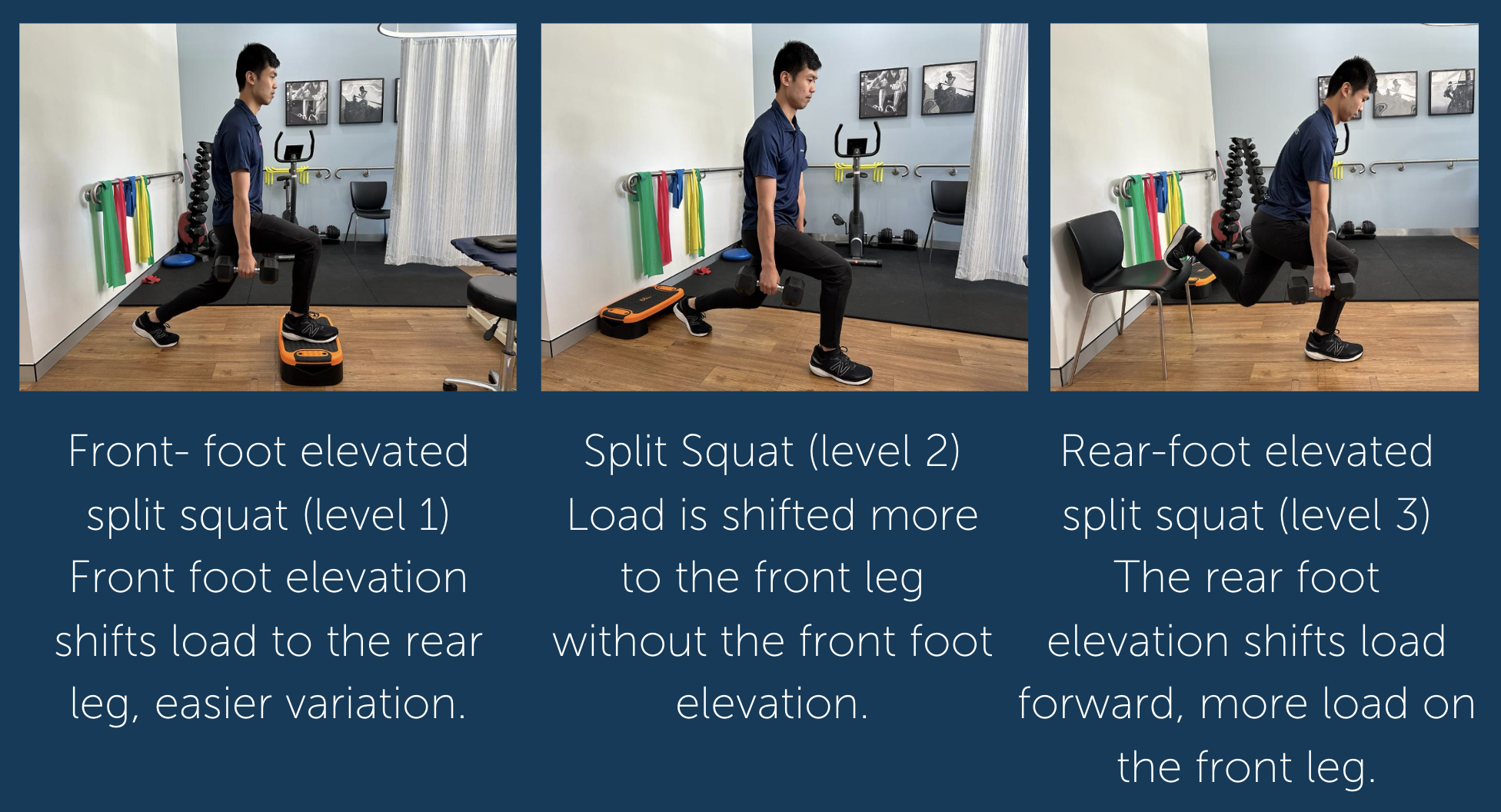
Split Squat Variations
Here are three split squat variations that are in order of difficulty, ideally you would pick the hardest variation you can tolerate. If pain worsens the following day with this program, use an easier variant.
Front- foot elevated split squat (level 1) – Front foot elevation shifts load to the rear leg, easier variation.
Split Squat (level 2) – Load is shifted more to the front leg without the front foot elevation.
Rear-foot elevated split squat (level 3) – The rear foot elevation shifts load forward, more load on the front leg.
There is evidence suggesting isometrics for tendons creates an immediate pain-relieving effect, this can be very useful for in-season athletes dealing with patellar tendinopathy. The above protocol can be useful short-term strategy to use pre-game/pre-training to elicit some pain relief so you can continue training and playing your sport.
The long-term goal would be to progressively add load to these isometrics, increasing sets/hold time and then transitioning to isotonic and plyometric exercises to further elicit an increase muscle and tendon strength, as well as store and release capabilities of the patellar tendon.
Conclusion
Patellar tendinopathy is always a load tolerance issue; thus, management should always address your current training loads and the load tolerance of your tendons. Isometric exercise is a fantastic entry point to improving load tolerance, eccentric and heavy slow resistance exercise are very useful progressions if well tolerated.
The resolution of symptoms can vary significantly depending on a range of factors including current training loads, severity of symptoms, age, general health and fitness, smoking/alcohol intake, biomechanical factors and psychosocial factors.
To get a complete rehabilitation plan that addresses your personal goals, I recommend all individuals see one of our physiotherapists or exercise physiologists who are highly qualified to manage this condition and get you back to the activities you love without pain.
References and additional resources
Patellar Tendinopathy: Clinical Diagnosis, Load Management, and Advice for Challenging Case Presentations | https://pubmed.ncbi.nlm.nih.gov/26390269/
Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy | https://bjsm.bmj.com/content/49/19/1277
Jumper’s Knee: 61 Things I’ve Learned [Fix Patellar Tendon Pain] | Jumper’s Knee: 61 Things I’ve Learned [Fix Patellar Tendon Pain] — JACKED ATHLETE
Effects of isometric, eccentric, or heavy slow resistance exercises on pain and function in individuals with patellar tendinopathy: A systematic review | https://pubmed.ncbi.nlm.nih.gov/29972281/